Cancer of the esophagus claims more than 400,000 lives around the world each year. With no efficient, reliable method of screening for the disease, by the time symptoms become apparent, it’s often too late to save the patient.
A Johns Hopkins researcher who has devoted his career to the detection and prevention of esophageal cancer today published a paper in the journal Clinical Cancer Research that he says could finally result in simple and inexpensive screening for the deadly disease.
In the article, gastroenterologist Stephen Meltzer, a professor of medicine and oncology at the Johns Hopkins University School of Medicine, along with a team of researchers, clinicians and biomedical engineers describe a test, the “EsophaCap,” that uses specific genetic biomarkers to detect dangerous changes in the cells that line the inside of the esophagus.
Previous studies have demonstrated Meltzer’s biomarkers’ ability to detect a condition called Barrett’s esophagus, which causes the body to replace the tissue that lines the organ with cells that can turn cancerous.
But large-scale methods to deploy those biomarkers as a screening tool have been elusive until now.
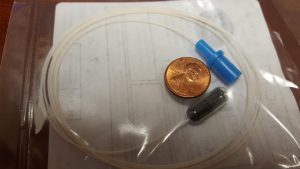
The principle behind the EsophaCap is simple, said Meltzer. The patient swallows a small capsule that has a long string attached to it. After the capsule makes its way down the esophagus and into the stomach – a process that takes only a minute or so – the gelatin coating on the capsule begins to dissolve.
From that capsule emerges a 2-centimeter polyurethane sponge, still attached to the string, much of which still hangs from the patient’s mouth.
The screener gently pulls the string and the sponge begins its return journey, out of the stomach, into the esophagus and, finally, out of the patient’s mouth.
As it makes its way up, the sponge comes into contact with the entire length and breadth of the esophagus, collecting genetic material all along the way. Then, as the sponge nears the top, the screener gives a final gentle tug, popping the sponge past the organ’s upper sphincter muscle. The sponge emerges loaded with genetic material that holds the key to the patient’s esophageal health.
The sponge is then sent to a company that performs simple genetic tests on the material to determine the patient’s risk for esophageal cancer.
“Early detection is the whole ballgame when it comes to esophageal cancer,” Meltzer said. “Patients have a much better chance to treat it–or even prevent it–if they know their risk. We believe this little sponge can bring easy and inexpensive screening to people around the world.”
With nearly half a million new cases a year, esophageal cancer is the eighth most-common cancer worldwide, with the highest rates in parts of Africa and Asia.
In 2016, the United States saw nearly 17,000 new cases diagnosed and about 16,000 deaths from cancer of the esophagus. Those numbers have increased sharply in recent years.
The five-year survival rate for people with cancer confined to the esophagus is 43 percent. When it spreads to nearby tissues or organs, that rate falls to 23 percent. And esophageal cancer that spreads to distant parts of the body offers a five-year survival rate of only 5 percent.
In previous research, Meltzer has performed rigorous testing on the set of genetic biomarkers he uses to diagnose Barrett’s esophagus. The gene combination of p16, NELL1, AKAP12 and TAC1 has yielded a sensitivity of nearly 92 percent and has offered reliable diagnoses.
Medicine has never had routine screening methods for the disease. Both endoscopy and biopsy are less-than-ideal, since they’re inexact, expensive and rely on random tissue samples, rather than material from the whole esophagus lining.
“It’s actually possible to miss early cancerous cells using endoscopy with biopsy and most patients with Barrett’s don’t ever undergo endoscopy,” said Meltzer. “Right now, we’re confident that we have the tools to identify this type of cancer. But we previously lacked a way to collect enough genetic material to confidently determine a patient’s diagnosis. We believe that EsophaCap now provides a solution to this serious problem.”
Meltzer administered the EsophaCap test to 94 people over the course of the study. Eighty-five percent of subjects were able to swallow the capsule, with 100 percent successful sponge retrieval. Endoscopic evaluation of the patients after EsophaCap administration, Meltzer reported, showed no evidence of bleeding, pain, trauma or other adverse reactions to the test.
In the journal article, Meltzer reports that of the patients able to swallow the capsule, nearly half would be diagnosed with Barrett’s esophagus–a rate far higher than that of the general U.S. population. He notes that most patients enrolled in the study were being treated for gastrointestinal symptoms.
“That may explain why we saw a rate of Barrett’s esophagus that was higher than in the general population,” he said.
Source: Johns Hopkins Medicine
Test for esophageal cancer could save millions of lives
74
SHARES
1.2k
VIEWS
Leave a Reply Cancel reply
Browse by Category
Tags
AAMI
AORN
Award
Bacteria
BIOCHEMISTRY
biology
cancer
CBSPD
Chemotherapy
colon cancer
colorectal cancer
colorectal cancer screening
COVID-19
Diagnostics
Duodenoscope
Education
EndoChoice
EndoPro Magazine
Endoscope
Endoscopy
FDA
gastroenterology
gastrointestinal disorders
Genetics
Healthmark
Hospitals
IAHCSMM
IBD
IBS
Infections
irritable bowel syndrome
MEDICINE/HEALTH
News
Olympus
Pentax
PHARMACEUTICAL CHEMISTRY
PHARMACEUTICAL SCIENCE
polyps
PPE
Public Health
recall
Screening
SGNA
Studies
Super Bugs
© 2023 Copyright. All Rights Reserved. Design & Developed by Insightful Technologies.