I may be dating myself here, but I remember when ethylene oxide (EO) sterilization was a daily occurrence in my sterile processing department (SPD). Why did that change? In short, EO is seen as a risk with little reward.
However, EO sterilization has continued to advance since the ’60s and ’70s, and while there are still risks, updates to the delivery technology, EO’s materials compatibility, and penetration capabilities mean there are rewards to the modality that you should consider. To fully understand whether EO could be a beneficial tool for device-processing facilities, we need to know its history and how it works.
Ethylene oxide was first utilized as an insecticide over 100 years ago. It wasn’t used as a sterilant for medical devices until 1950. Interestingly, that was two years after EO was discovered to be a mutagen. Even so, EO’s broad compatibility, ability to penetrate various packaging materials, and long lumens made it a viable option for sterilizing a wide range of heat-sensitive medical devices. It wasn’t until 1986, when a major disaster in India killed thousands, that the deadly risks of large-scale EO sterilization became undeniable.1
Still, EO continued to be utilized as an effective sterilant, so its effects on the human body continued to be studied. California officially declared ethylene oxide to be a human carcinogen in 1987. Around the same time, the National Institute of Occupational Safety and Health (NIOSH) declared that EO could cause breast cancer and lymphomas. With such an infamous history, one might think EO sterilization never made it out of the 1980s. But it absolutely did.
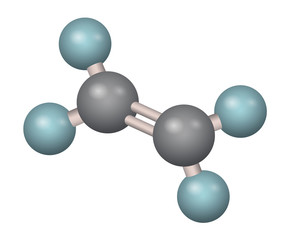
How Ethylene Oxide Works
EO sterilizes through alkylating of proteins, DNA and RNA of microorganisms, replacing an alkyl group where a hydrogen atom would be. When this happens, the cell’s normal metabolism and reproduction pathways are disrupted. To be effective, EO sterilization requires four main components: a) adequate gas concentration, b) correct temperature, c) a specific relative humidity, and d) the correct exposure time. Combining all four factors in the proper amounts produces a sterile device. However, the process also often requires long cycle times—between 12 and 24 hours when including aeration. Cycle time can be shortened by increasing the temperature and concentration of the gas, but at a potential cost of affecting the materials the device is made of.
With clear risks to humans and its long cycle time, why would we continue to use EO, especially in a hospital setting? The answer is simple: The rules in place to protect workers and the environment during small-scale sterilization are effective. Hospitals utilizing older EO technologies were required to isolate the area entirely by dedicating a room to it, keeping that room under negative air pressure, and having specified air-exchange rates. They were also required to monitor the area for leaks and store tanks and canisters of EO in specific conditions.
Today, those same safety requirements are some of the reasons EO sterilization seems cumbersome and not worth the large amount of real estate it consumes. Factoring in the size of the sterilizers, the abator (the engine for burning off the EO gas), and tank or canister storage, an EO room could easily take up 200 square feet, if not more.
Space concerns are not the only factors that cause people to wince when considering EO. In older versions of EO delivery technologies, the gas concentration needed to be high. This created staff and environmental concerns with EO sterilization. When it comes to staff safety, the Occupational Safety and Health Administration (OSHA) has well-defined exposure limits for working with EO. Facilities are required to monitor staff members periodically when working directly with the gas—generally annually, if not more frequently, for exposure. These excursion limits are measured in a time-weighted averages (performed on short, 10- to 15-minute intervals and a more extended, eight-hour timeframe).
Along with testing employees, the amount of ethylene oxide gas released into the environment must also be measured. Older EO systems needed higher concentrations of gas to be effective, so a method to reduce the amount of EO released to the outside was required. This is done by an abatement process. Abators are large units hooked into the exhaust line, often using heat, to convert excess EO into CO2 and water vapor, which can then be safely released into the environment.
With all this said, how can EO be seen as anything but a risk to facilities, and what possible reward could there be for utilizing it in a facility? Answer—a higher margin of patient safety over high-level disinfection (HLD). That margin lies between the level of microbial destruction achieved in HLD versus sterilization. These stringent requirements and long cycle times led many to believe that sterilization of flexible endoscopes was not an option.
In 2015 duodenoscopes made the news in a bad way: they were linked to carbapenem-resistant Enterobacteriaceae (CRE) outbreaks that caused multiple patient deaths. Because of their design, these endoscopes presented a processing challenge to facilities that utilized them.
Proposed Solutions
The United States FDA and CDC responded by providing guidance that supplemental processing steps for endoscopes with elevator mechanisms could be utilized. These additional steps included repeat high-level disinfection, liquid chemical sterilization, and low-temperature sterilization. These measures were meant to increase the margin of safety for patients. It was later discovered that double-HLD was ineffective in improving this safety margin; however, the sterilization methods did demonstrate effectiveness.
Why? Two factors.
- If the devices were not or could not be adequately cleaned, none of the following disinfection or sterilization processes could be as effective. Still, high-level disinfection was even less effective because HLD does not kill high numbers of bacterial spores. So, repeating the process twice made little difference.
- On the other hand, sterilization offers the destruction of all forms of microbial life.
So why not sterilize all flexible endoscopes, or at least the models with the most complex designs?
One answer lies in the interpretation of the Spaulding Classification, a hierarchy for the level of disinfection or sterilization required to render reusable, patient-care devices safe for the next patient. Created by Dr. Earle H. Spaulding more than 30 years ago, the classification is still considered the most rational approach to making this distinction. According to Spaulding, flexible endoscopes are generally classified as semi-critical devices (depending on intended use), indicating they contact intact mucus membranes or nonintact skin but do not enter sterile tissues. Because of this, they can be subjected to sterilization but, at minimum, high-level disinfection if sterilization is not an option.
Those outbreaks sparked a debate about the benefits of sterilizing flexible endoscopes. This prompted changes to standards guidance—from organizations like the Association for the Advancement of Medical Instrumentation (AAMI)2 and The Association of Operating Room Nurses (AORN)3—to stress that HLD, while acceptable, is the minimum processing level, but sterilization is preferred.
It’s easy to understand the push toward sterilization. Many patients undergoing a procedure like endoscopic retrograde cholangiopancreatography (ERCP) or various bronchoscopy procedures are already considered compromised and at increased vulnerability for infection. If this is the case, why aren’t all flexible endoscopes sterilized? Unfortunately, the most complicated (and therefore the most difficult to process) flexible endoscopes possess channels that are either too long or too narrow for many low-temperature sterilization modalities, such as vaporized hydrogen peroxide (VH2O2). There are also material compatibility concerns with VH2O2 that could drastically shorten the scope’s useful life (or ruin a scope entirely), adding to the reasons many believe that high-level disinfection is the best option for their endoscopes.
If your understanding of EO sterilization is what I have described in this article so far, I can understand why you feel HLD is the only option, but now I will attempt to change your mind.
You must be thinking, What does Seth want me to do, wave a magic wand and come up with space and equipment to sterilize all my flexible endoscopes? No, but before you give up on the idea, know that some facilities are already pushing to make this a reality. I worked in a facility that invested in the equipment and the increased inventory of endoscopes needed to sterilize all flexible endoscopes that came to the SPD. The list of endoscopes we were responsible for included flexible rhinoscopes, cystoscopes, ureteroscopes, and three models of bronchoscopes. In case you are wondering, all duodenoscopes were sterilized using EO after 2015.
I know what you’re thinking. Of course, you were able to do that; you were in an SPD area with space and resources. While we did have more space than a typical endoscopy clinic processing room, we still needed to procure other resources that were not space-related. This was done through collaboration with multiple departments and spearheaded by infection prevention. It took several planning meetings, required us to consider all aspects of scope reprocessing (from the point-of-use treatment to the storage space for sterilized endoscopes), and develop a budget and timeline for implementation. It was not an easy process, but the quality it added to our scope processing program was deemed worth the effort. I am not saying centralizing your flexible endoscope processing is the only way to accomplish the goal of sterilizing endoscopes, and my example does leave out the one thing that cannot be easily planned for or purchased: space.
What if I told you that space did not have to be as big an obstacle as it used to be? It is now possible to EO sterilize endoscopes in an area not much bigger than a table-top sterilizer and with few of the other infrastructure needs of older systems, too. This is where those advances in EO technologies come into play. As mentioned, ethylene oxide sterilization technology has not remained static over the last 60 years. As a matter of fact, the FDA has granted 18 Section 510(k) clearances for updated EO technologies (the most sterilizer clearances for any sterilization modality) in recent years. This is no small feat, given how sterilizer testing is done and the complexity of flexible endoscopes.
When clearing a piece of equipment, such as a sterilizer, the FDA requires worst-case scenario testing. However, after 2015, the FDA took a hard look at duodenoscopes and decided they were not a single instrument, but multiple instruments working together. Working with this concept, the FDA required sterilizer manufacturers to inoculate eight worst-case scenario points on these scopes (instead of a single point), then prove their sterilizer could effectively reach those areas. This is where the penetrating power of EO shows its efficacy again. Its ability to make its way down narrow, long lumens and into small spaces made it ideal for reaching all these areas.
What is new for EO sterilization? These sterilizers are now tested to a very high standard of effectiveness, and the space requirements have been dramatically reduced. One sterilizer manufacturer developed a system using a flexible sterilization bag placed inside a small cabinet under negative pressure. This system requires very little space. The cabinet itself is kept under negative pressure, eliminating the requirement for isolating an entire room. The sterilizer manufacturer’s update to abatement methods is also a considerable improvement. Using a cationic resin means almost no EO is released into the atmosphere.4
In my opinion, the most significant leap forward is that they reduced the concentration of EO gas needed for sterilization while also decreasing the cycle time. Updated EO sterilizers can use orders of magnitude less gas than previous versions, with their system only requiring 17 grams of EO per cycle, while simultaneously bringing cycle times down to between three and six hours, depending on the length of the lumen being sterilized. This reduction in gas concentration and time means the entire system can be smaller, simpler and more cost-effective.
To be clear, even with these advances, staff and area monitoring are still necessary when using ethylene oxide. However, this monitoring may also be required for other sterilization and HLD methods. The system still requires venting to the outside, but gone is the need for water lines, fully isolated, negative-pressure rooms, and large abators.
The last point I want to make is about price. I know it’s easy to say, “Quality doesn’t cost. It pays.” While I do believe that’s true, it is also said, “Money doesn’t grow on trees.” Any practical sterilization solution must also consider the budget constraints we all face. Again, updated EO technologies have a benefit to offer. Advancements have reduced the size, materials and space needed for one of these sterilizers, while reducing the cost. It is possible to get a new sterilizer for around $50,000. For perspective, that is less than one-quarter of the price of most VH2O2 sterilizers.
Have I changed your mind about EO? In researching this article, my mind was changed. Even though I was aware of many of these updates to the modality, I couldn’t get the image of an outdated EO room out of my head. Now all I see when I think of ethylene oxide are possibilities. The possibility that pushes toward sterile endoscopes is attainable and not just a recommendation to be dismissed. This means the most vulnerable patients can receive needed treatments with these devices with the highest margin of safety possible, and we may be able to stop another outbreak—without going broke.
Increasing quality and patient safety when utilizing flexible endoscopes should be an ongoing process that receives review and revision. At your next risk-analysis meeting, consider that flexible endoscopes can be EO sterilized in a way that is space-efficient, cost-effective, and safe for patients, staff and the environment. Those sound like rewards worth exploring.
Seth Hendee is a clinical education specialist with Healthmark Industries, Inc.
References
- Hawthorne, Michael. (October 16, 2019). “From Discovery of a Powerful Chemical to Shutting down Sterigenics: 160 Years of Ethylene Oxide.” Chicago Tribune. https://www.chicagotribune.com/news/ct-sterigenics-eto-timeline-htmlstory.html
- ANSI/AAMI ST91:2021. Flexible and semi-rigid endoscope processing in health care facilities. American National Standard. Association for the Advancement of Medical Instrumentation. Arlington (VA).
- Association of perioperative Registered Nurses (AORN). Guideline for cleaning and processing flexible endoscopes and endoscope accessories. Guidelines for Perioperative Practice. AORN, 2018e
- “Emissions Abators.” (12 May 2022). Andersen Sterilizers. https://www.sterility.com/gas-abatement-equipment-eto-abator-sterility/.